Leveraging Workforce Data
Figures on anticipated physician demand, a rapidly aging population, and geographic maldistribution illustrate why comprehensive, statewide strategies to address workforce needs are necessary today. Changes in care delivery, such as Accountable Care Organizations (ACOs), telehealth, and team-based care also shift how the workforce is utilized. What data sources are instrumental in understanding workforce demands both today, and in the future? Further, what does the data suggest is needed to address these demands?
Regional Shortage Projections
WCMEW’s 2018 workforce report, Mapping Our Way to Success, identifies Wisconsin Hospital Service Areas (HSAs) with projected primary care physician (PCP) shortages. According to the report, demand for primary care is projected to increase by 20.9% statewide, although there is wide variance among HSAs, ranging from 3.9% to 39.7%. Total population increases, together with an aging population, are drivers of increases in demand. Statewide, there is a projected shortfall of 745 FTE PCPs, or 14% compared to overall supply. Wide variance among HSAs is evident, ranging between a surplus of 24.4% and a deficit of 93.7% – as indicated in the map to the left. Dark orange areas indicate highest unmet need. Rural communities are expected to see the greatest percentage deficits, whereas metro areas can expect the greatest total FTE deficits. Data shows that while the population is expected to increase 12% statewide, demand is expected to increase by over 20%. Supply of PCPs is projected to increase by approximately 4%. The 2018 report includes additional data and figures for today’s total physician workforce, including specialty and practice location.
supply and demand
WCMEW's 2016 workforce report, A Work in Progress: Building Wisconsin’s Future Physician Workforce, evaluates multiple scenarios related to statewide physician supply and demand in Wisconsin. If clinician "lifestyle" changes (including preferences for increased work-life balance, and changing demographics) are included in projections, the supply of physicians is estimated to decrease. While demand (based on overall population growth, and an aging population) will increase regardless, demand is expected to increase less sharply with reforms such as team-based are and increased use of telehealth services. WI's Physician Workforce Profile, courtesy of the AAMC, is also available here.
clinician maldistribution
Physician demand varies across the state, and the impact of shortages is felt more acutely in rural areas, along with parts of Milwaukee. Other maps for psychiatry and dentistry show similar trends. Various initiatives such as WARM, TRIUMPH, and new Medical College of Wisconsin campus locations aim to address workforce needs in targeted areas.
Health Professional Shortage Area (HPSA) maps are available for primary care, dental, behavioral health, and the Milwaukee metro area.
Map courtesy of the Wisconsin Office of Rural Health, with the Wisconsin Office of Primary Care
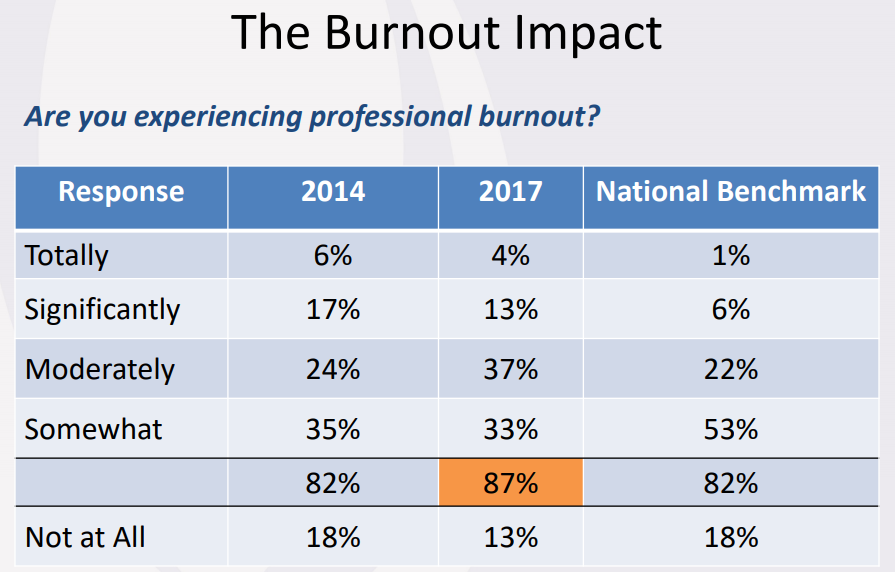
Provider Burnout
In 2018, The Wisconsin Medical Society completed the second installment of assessing satisfaction levels for Wisconsin physicians. The study found that over half of practicing physicians describe being burned out or having symptoms, higher than national benchmarks. 2017 data also shows that 45% of physicians will plan to reduce clinical hours or retire in the next 5 years, up from 42% in 2014. While burnout is not experienced solely by physicians, the impacts can be widespread, affecting rates of medical errors and quality of care.
Data courtesy of the Wisconsin Medical Society
aging population
One particular workforce factor that contributes to a pressurized health care system is Wisconsin's aging population, exacerbated by relative stagnation in working age population growth rate. In 2010, 19.2% of Wisconsin's overall population was age 60 and over, compared with a projected 29% in 2040. Further, some counties, including Adams, Bayfield, Iron, Marquette, and Price are expected to see nearly half of their population age 60+ by 2040.
Maps courtesy of Wisconsin Hospital Association 2017 Workforce Report, DOA Data
workforce retention
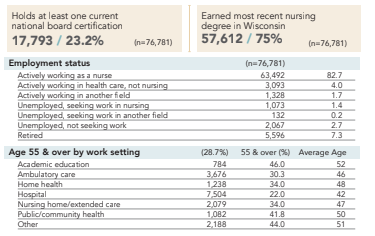
The Wisconsin Center for Nursing collects gold-standard re-licensure nursing data for RNs and LPNs, in alternating odd and even years. This data shows that over one-third of Wisconsin nurses plan to leave direct patient care within the next decade. Similarly, one-third of current active physicians nation-wide will be 65 or older in the next 10 years. Maintaining adequate academic faculty to train the next generation of nurses is key to supporting a sufficient nursing workforce. Nursing faculty shortages is an area of concern, as nearly half of all current nurses in an academic setting are age 55 or older.
Data courtesy of the Wisconsin Center for Nursing
Aging Professions
The Wisconsin Hospital Association conducts an annual analysis of health profession data across the state. WHA’s 2018 report lists LPNs, Lab Technologists, and CRNAs as the oldest workforce groups, with PAs among the youngest.
Data courtesy of the Wisconsin Hospital Association
care delivery and payment reform
WCMEW's 2016 Report developed projections based on multiple care delivery scenarios, including increased use of telehealth and team-based care. In addition, payment reforms, such as utilization of Accountable Care Organizations (ACOs) will also impact the health care workforce. Telehealth utilization is on the rise nationwide (see utilization chart), for both commercial and Medicare beneficiaries. The net effects of telehealth are yet undetermined, but potential impacts cannot be ignored for the health care workforce and patient access to care.
Chart courtesy of Milliman